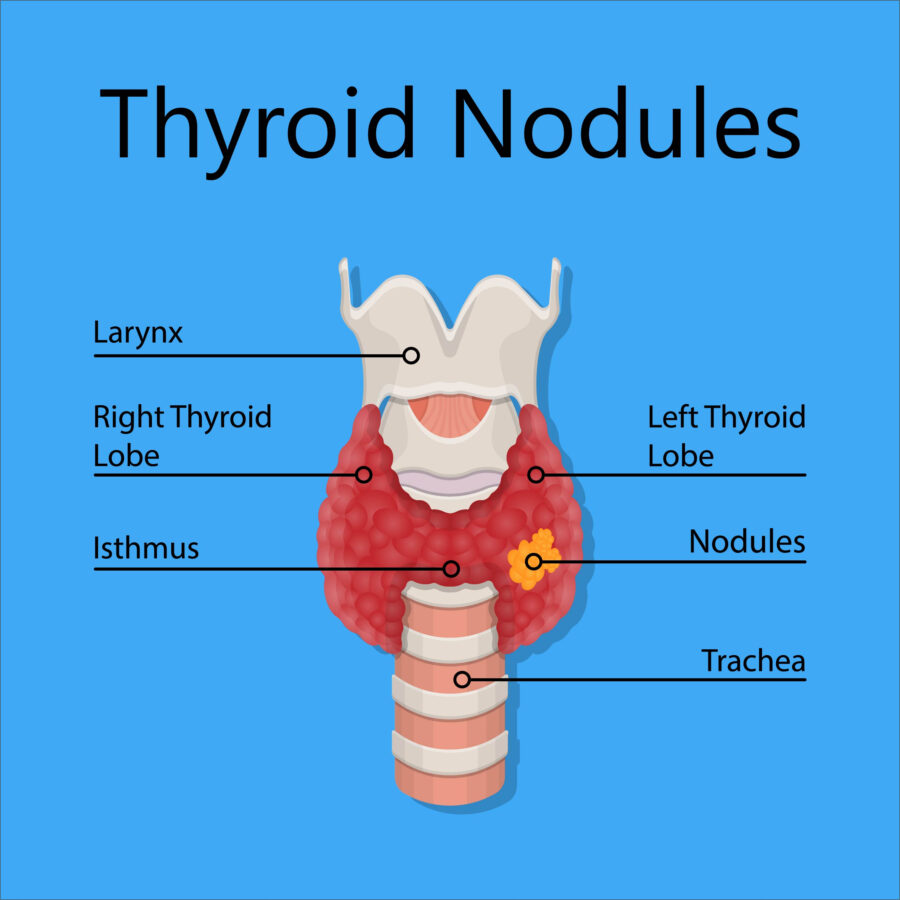
What is a thyroid nodule?
A thyroid nodule is an area of thyroid tissue that has developed abnormally. It can be solid or liquid (cystic). Typically, most nodules are benign, although they should be evaluated for cancer if the ultrasound suggests the need. Thyroid nodules come in varying sizes. Some may cause alterations in your thyroid hormone levels. Occasionally they present with symptoms of pressure, compression, or hoarseness.


